Nurse Practitioner Documentation Template

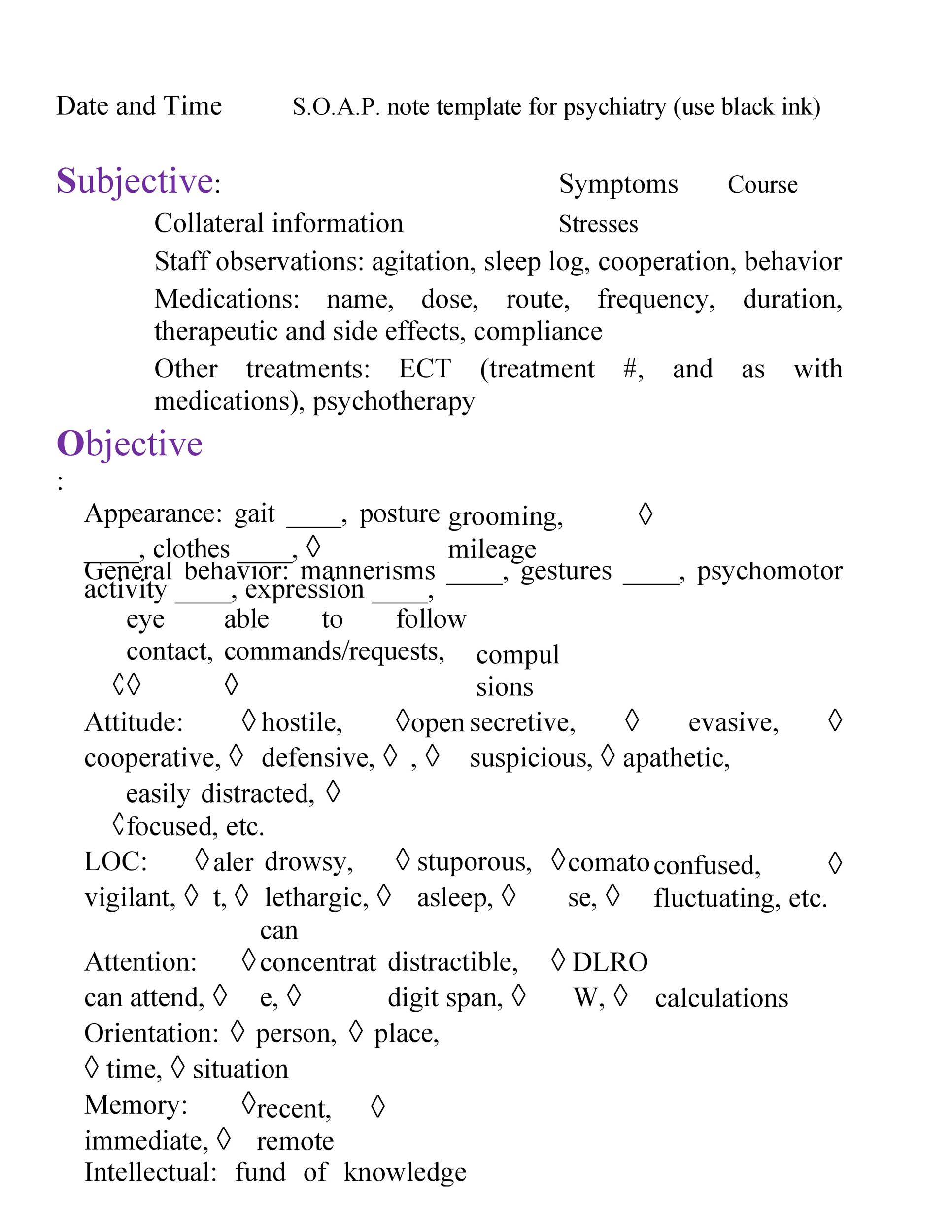
Soap notes are a type of documentation which when used help generate an organized and standard method for documenting any patient data.
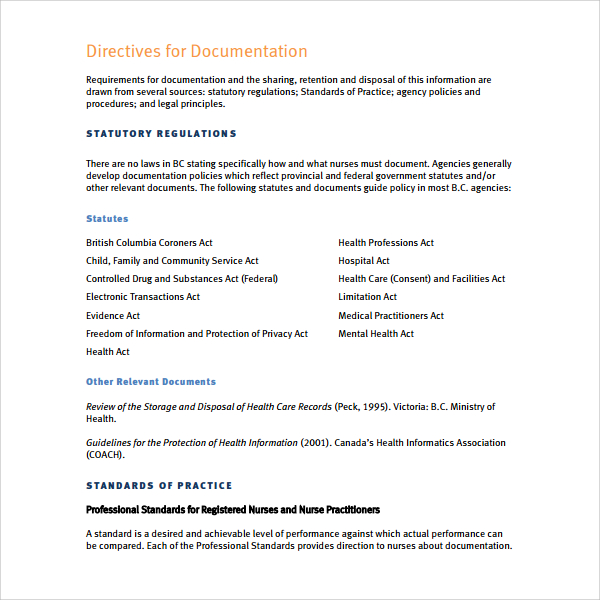
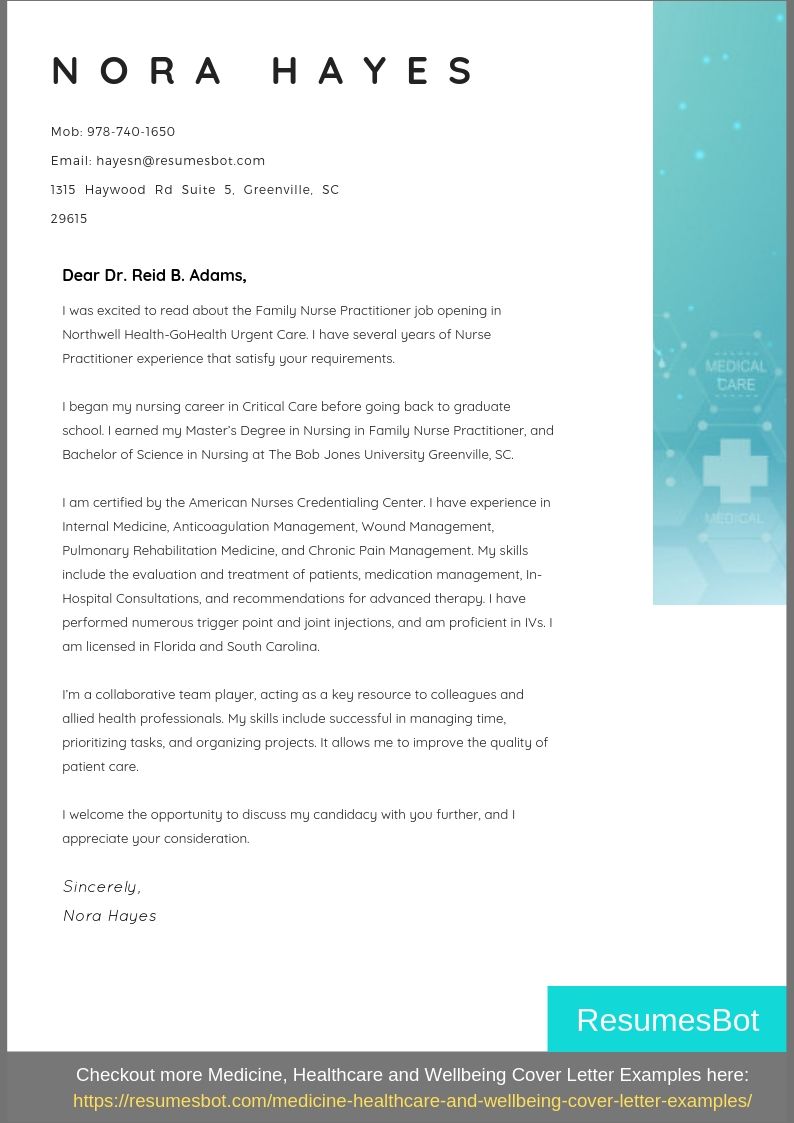
Nurse practitioner documentation template. The purpose of this progress note is to assist the physician andor medicare allowed non physician practitioner npp in documenting patient eligibility for the medicare home health benefit. Helpful hints and tips within the templates can improve patient care and save time. To prevent those kind of scenarios we have created a cheat sheet that you can print and use to. The delegating physicians must determine what medical acts heshe will delegate.
What youre looking for. All parties to the paa should participate in the development. Each will address the problems from a wide variety of professional perspectives. A psychiatric assessment may occur at any time during the course of treatment for the purposes of diagnosis treatment planning medication therapy andor consideration of general health issues.
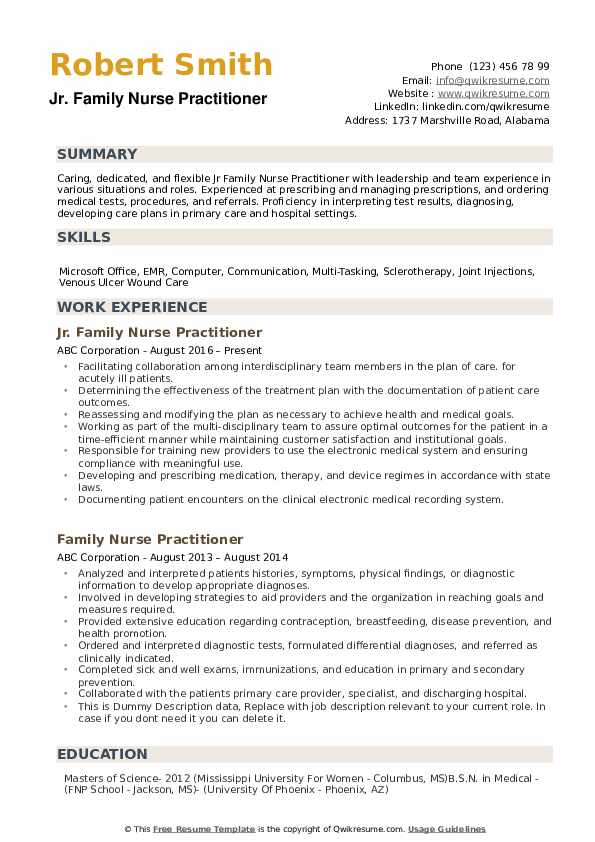
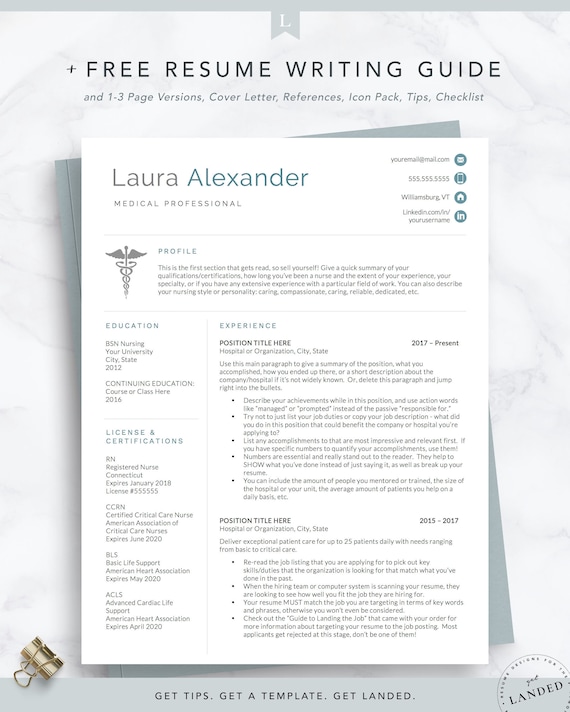
As a nurse practitioner you likely treat the same or similar medical conditions on a repeated basis. In addition templates can be customized to your practice style with reminders and content through our system. With a weak or incorrect assessment nurses can create an incorrect nursing diagnosis and plans therefore creating wrong interventions and evaluation. Assessment can be called the base or foundation of the nursing process.
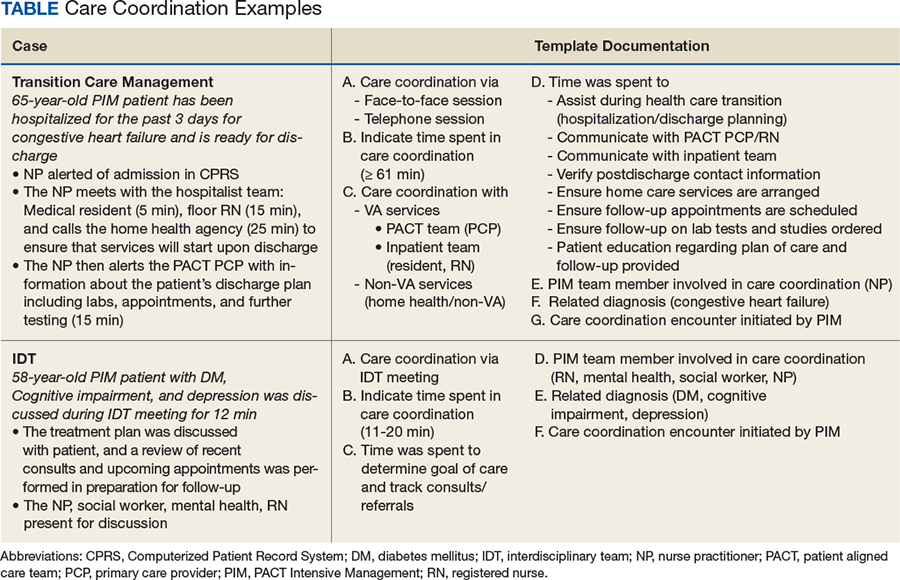
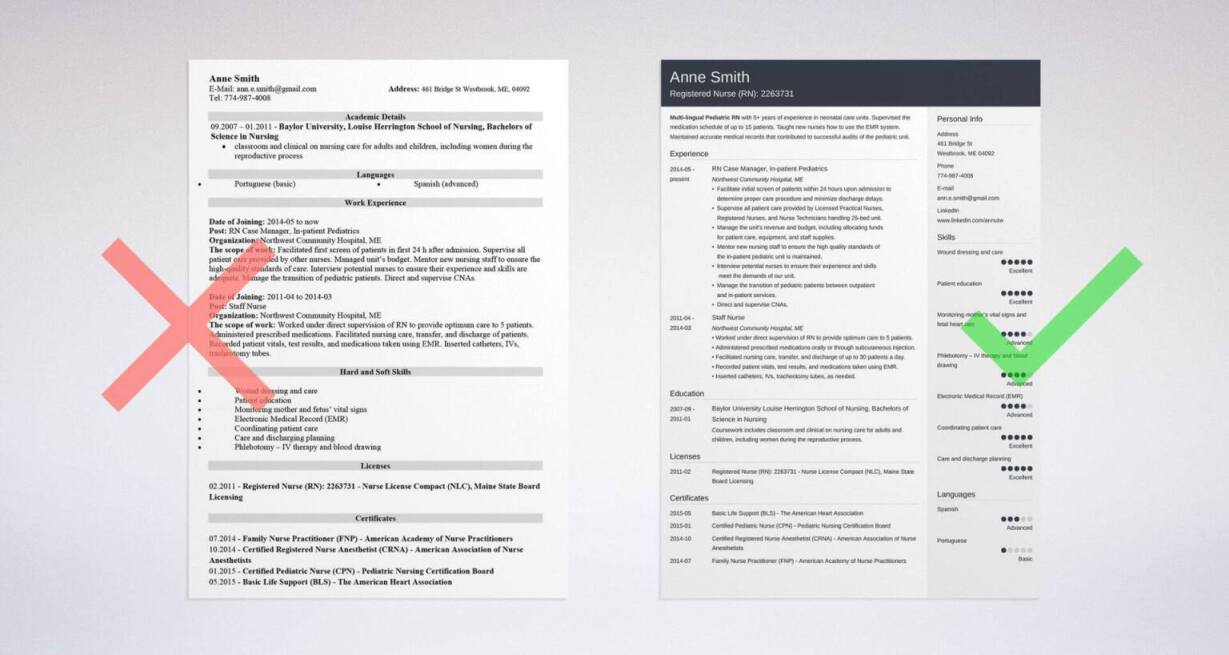
Progress note guidance. Any type of health professionals can use a soap note template nurse practitioners nurses counselors physicians and of course doctors. Create documentation templates for the most common conditions you diagnose. This way the next time you diagnose a patient in your pediatric clinic with strep for example your chart is nearly complete with the click of a button.
Health care practitioner physical assessment form this form is to be completed by a primary physician certified nurse practitioner registered nurse certified nurse midwife or physician assistant. Whether youre doing a well child check up or assessing a patient for an acute illness as a nurse practitioner youll likely do your fair share of heent exams and must be familiar with the exams basic components. It may be done more frequently if needed. A variety of different professionals practicing in a given institution might be writing soap notes on a patient.
Nursing assessment is an important step of the whole nursing process. This document can be placed in the progress notes section of the patients medical record. Psychiatrist or nurse practitioner in psychiatry or physician assistant with specialized training approved by the office. The document should be reviewed signed and dated at least annually.
The dietician may address the patients compliance or comprehension of an ada diet and document the visit in the form of a soap note. Our note templates provide blocks of patient documentation that can be inserted into any note in any emr.