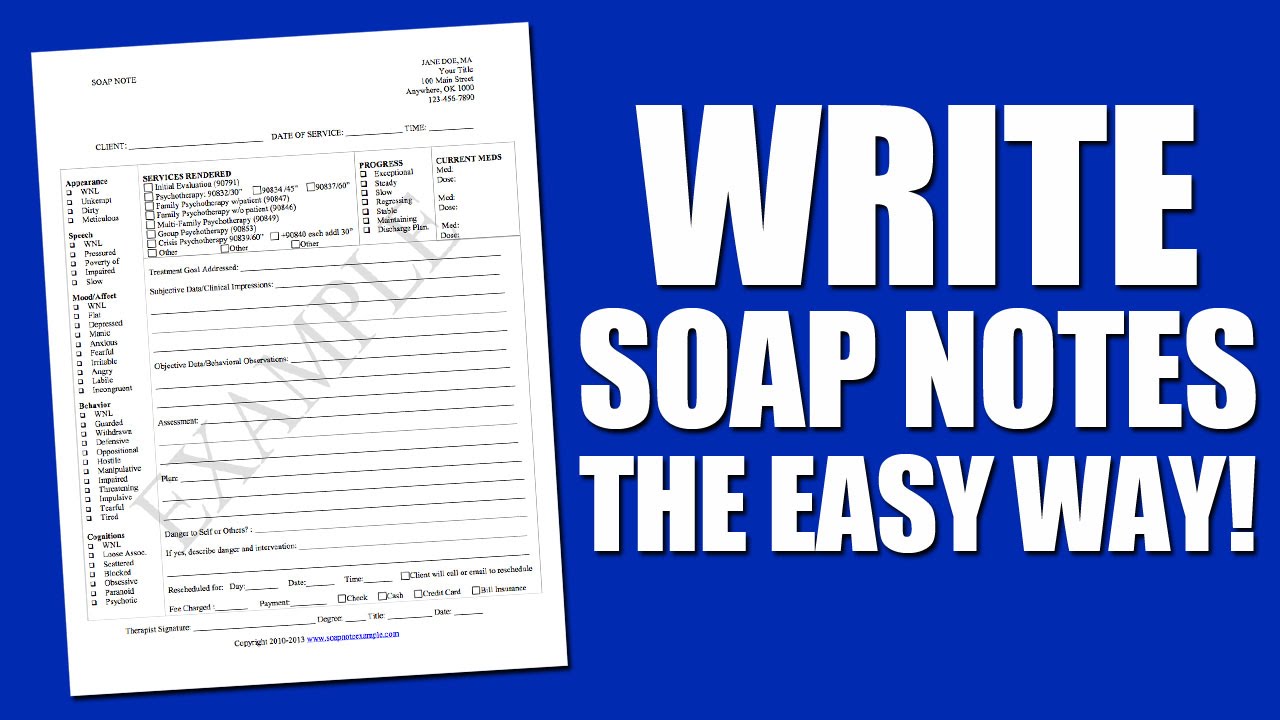
Sample Soap Note Template

These free notes templates lengths usually differ but in most cases they are brief.
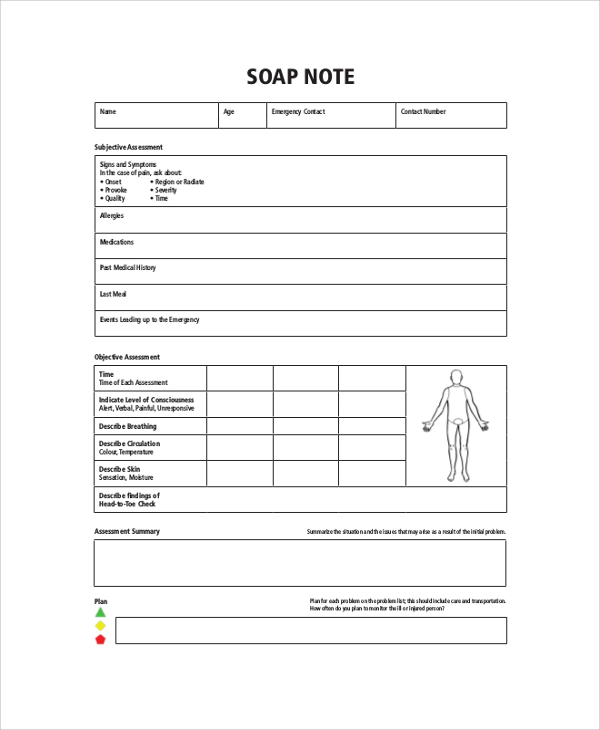
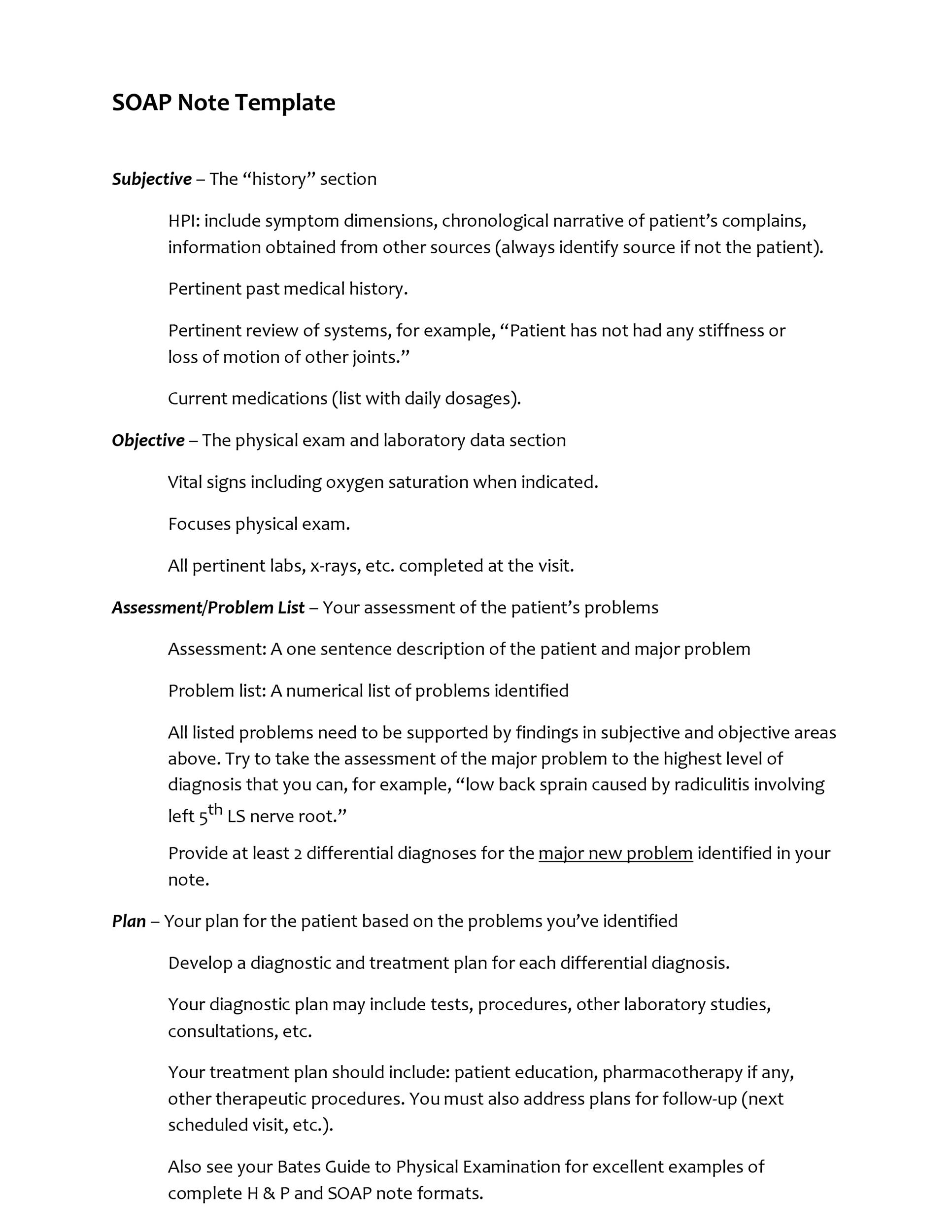
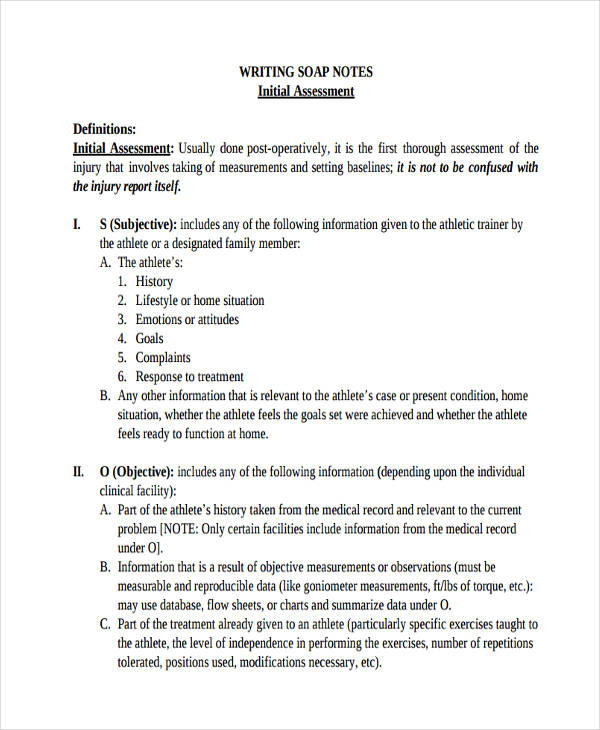
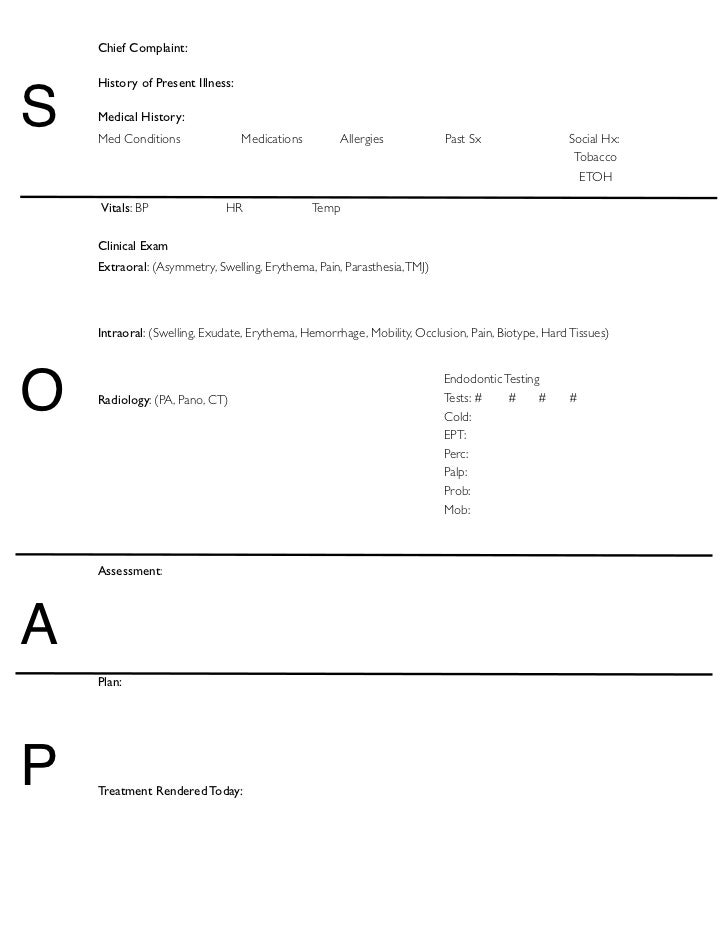
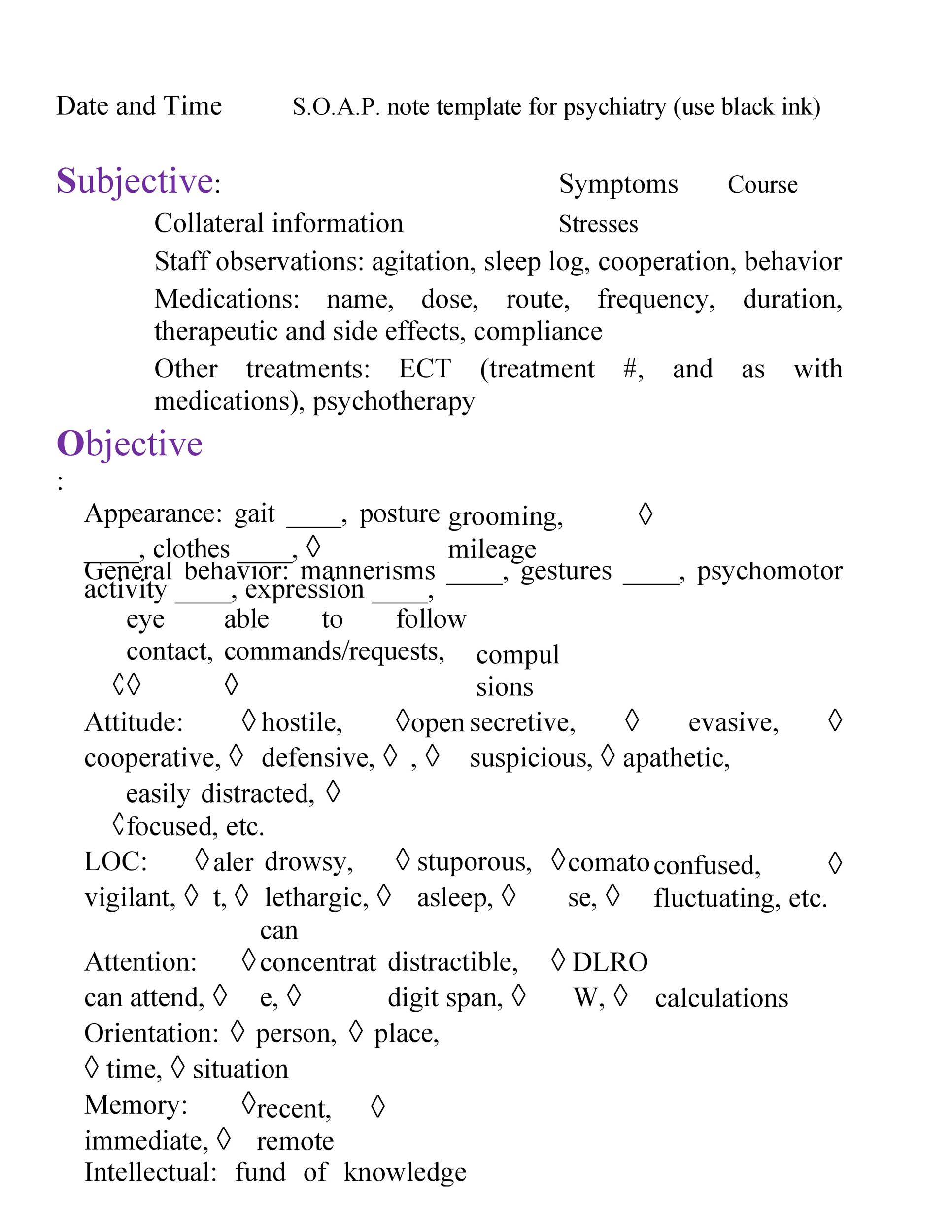
Sample soap note template. Download free soap note example here. A soap note template comes in a very structured format though it is only one of the numerous formats health or medical professionals can use. Download the sticky note templates as they come in easy accessible word excel format. The soap notes template is an easy and an effective method for quick and proper treatment for a patienta soap note is usually made up of four divisions the subjective part that has the details of the patient the objective part that has the details of the patient.
The soap note templates are extensively used in the medical fields. The patient is here today with a tick bite on his upper right anterior thigh. This is the part of. These soap notes are progress reports prepared to record the conversations between a medical practitioner and patients.
The patient presents in followup for his left. He removed it last night and notes that the tick was quite tiny. The four parts are explained as below. Developing a soap note.
More soap note samples. Soap note an acronym for subjective objective analysis or assessment and plan can be described as a method used to document a patients data normally used by health care providers. To ensure that a patient gets the perfect treatment hospitals often employ the soap analysis by writing down a sample soap note. Totally free soap notes templates.
Download these templates right now and start using. Subjective the subjective section contains a summary statement that is given by the client. A soap note template is a type of progress report usually prepared in a chart format. The templates have been fabricated attempting to know about the health of patients dealt with their present condition list of activities that they can schedule in their routine etc.
The sample soap note template has a number of characteristics. Sample soap note. Given below are a few sample statements which can be used while developing a soap note. This data is written in a patients chart and uses common formats.
These include objectives assessments plans and subjective are among the four main components of a soap note.